|
·
The easy availability of mother’s
milk, its sterility, its temperature and its composition are ideal
for optimal growth. Breast-feeding supports the emotional
development of the child , through enjoyment of an essential and
privileged relationship with his/her mother. Mother’s milk is the
best food that can be offered to the infant from 0 to 4 months of
age ; breast-feeding can be continued for 1 to 2 years providing
that the child receives other necessaary foods;
·
The composition of breast milk
develops according to the infant’s needs for growth ; the
nutritional and immunological properties of breast milk are adapted
to the child’s needs;
·
The quantity of breast milk is
theoretically sufficient for the needs of the child unit the age of
4 to 6 months ; this depends on the effective stimulation of the
nipple by sucking and on emptying the breast. Errors in the
technique of breast-feeding, as well as malnutrition or a depressive
state in the mother; can suppress breast milk production.
PRACTICAL WAYS TO DEAL WITH BREAST-FEEDING
1.
Slow onset of lactation,
sometimes taking 4 to 5 days.
Sucking stimulus of the nipple
encourages the flow of the milk . The infant should be put to the
breast as early as the first hours of life; indeed any
colostrum it takes is nourishing and the smallest amount of sucking
will help stimulate milk production.
To increase the production of
milk , it is also necessary to:
·
feed the mother adequately;
·
encourage her to drink;
·
allow her to rest;
·
calm her and reassure her.
2.
Cracks in the nipple: small,
superficial but painful coetaneous lesions, caused by chronic
irritation or poor hygiene.
·
Prevention: clean
hands, washing the nipple with cooled boiled water , keeping the
nipple dry and covered.
·
Treatment: cleaning and
drying the nipples , and the application of a 2% aqueous solution
of eosin (not harmful for the infant).
· Because stopping sucking suppresses
lactation and causes painful engorgement of the breats and may cause
mastitis or breast abscess, it is essential to continue feeding.
This should be done by either continuing to offer the breast, or by
expressing the breast gently and regularly to empty it . The milk
can be given to the infant with a spoon.
3.
Mastitis: infection of the
mammary gland.
Early
sings: swelling, heat and reddening , local or diffuse ; pain,
sometimes considerable.
Treatment:
·
Wrapping in cold or chilled
compresses;
· anti-inflammatory
drugs (aspirin, 3
g/day in three doses for 48 hours);
·
(e.g.spiramycin, 3 g/day in three
doses for 7 days);
·
expressing the affected breast gently
and discarding the milk;
·
continuing to offer the other breast
to the infant.
4.
Abscess: a collection of pus in
the mammary gland.
Clinical signs of abscess
formation: localised,very painful, hot and red.
Treatment: in addition
to the treatment for mastitis:
·
incision and drainage when the abscess
is fluctuant;
·
the infant can return to the breast as
soon as the abscess is cured.
5.
“My milk is not good” , or
“ I don’t have enough milk”, or “My child does not want
the breast any more”
Contraindications for breast-feeding are very uncommon and usually
temporary. Basides , a healthy child is hungry. If the mother says
that the child does not want the breast but “ accepts the bottle” ,
a reason must be sought.
Management:
·
explain the benefits of breast
–feeding to the mother and find out,without making her feel guilty
the reason for her choice,
·
if it appears that breast-feeding is
not possible find out:
-
if she has the material and financial means
necessary for artificial feeding (allow for 2 to 3 kg of mild powder
per month);
-
whether she is capable of correctly preparing
an infant formula;
·
if the child is ready for
supplementation (3 to 4 months ) or for introduction of
solids, recommend an adequate complementary food.
1
6.
“ My child is always at the breast”
or “ My child falls asleep whilst at the breast”
Simple
conditions must be met so that breast-feeding goes well:
·
the mother must be relaxed and
comfortable, either sitting or lying down , and wanting to feed her
baby;
·
the infant must be relaxed , not tired
, not satiated , nostrils clear, not pressed against the breast;
·
the nipples must be cleaned before and
after each feed;
·
the infant’s sucking reflex is
stimulated by introducing the nipple into its mouth and by
preliminary gentle stroking of the lips;
·
the breast should be gently squeezed
to produce a few drops of milk for the infant to taste, a maneuver
which will stimulate and maintain sucking and the letdown reflex;
·
the continuing secretion of milk
should be maintained by gentle squeezing of the breast; the infant
should be stimulated (e.g. by caressing, talking, singing and
looking);
·
in this way, the infant will have an
adequate meal , followed by a period of digestion , after which he
will wake up for the next meal. The frequency of feeding is
determined by the infant according to appetite, but for a term
infant there should be at least six feeds per day in the first
months; and there should be even more frequent feeds for premature
infants . The infant who sleeps too much should be awakened for
feeding; the more often he suckles, the more milk the
mother will have . sugar water from a bottle must not be given.
7.
“I must go to work” or “I
have to go to the market”
A mother’s social life and the economic needs of the
family sometimes cause a lactating mother to leave the house to work
or go to the market.
Sometimes she cannot or “will not” take her child with
her. Although she must be encouraged (many mothers feed on demand
and offer the breast whiled following their occupation), and although
the lactating mother must be spared the heavier takes, the health
supervisor may sometimes have to agree to an occasional artificial
feed , provided it is properly made up , according to the strict
rules of hygiene.
1. 1.
Choice of milk:
·
do not use milk which is not adapted
for infants;
· most infant milk formulas are suitable
for all infants; they consist of cow’s milk which has been
modified and enriched to satisfy the normal nutritional
requirements of infants and adapted to their physiological
characteristics.
Infant formula may also be prepared at home in
which case it is described as “home-prepared” (WHO International
Code of Marketing of Breast-milk Substitutes, Geneva1981).
2.
2.
Choice of water:
·
Clean drinking water will do , if
possible boiled and filtered;
·
Of the bottled waters, only those with
low mineral content are suitable.
3.
3.
Choice of feeding utensils:
·
as far as possible , use a cup
and spoon for easier cleaning;
·
glass feeding bottles (which can be
more reliably washed and sterilized) with simple and clear
graduation marks, preferably at 30 ml intervals;
·
bottles and teats should be carefully
washed and boiled for 15 minutes each time before use; they should
be sterilized in a pan or in a special sterilizer.
4.
Making up the milk:
·
it must be very carefully
prepared; the hands must be washed beforehand;
·
most tins of infant formula contain a
measure marked with its capacity (usually 4.5g).The measure should
be filled level , not heaped , say 4.5g in 30g water, 2 measures for
60g water, 3 for 90 g and so on;
·
put a little tepid water in the bottle
, add the measures of infant formula; shake to dissolve; than add
water up to the required amount;
·
carefully close the tin after use.
·
Remarks about the use of ordinary
milk powder : after making up according to the instructions on
the tin, it is necessary for infants up to 6 months of age to dilute
it by putting one part of water in the bottle and adding two parts
of reconstituted milk up to the quantity required; 5% sugar must
also be added
5.
Quantities of milk to be given:
·
Apert’s rule:
Total
quantity (ml) per 24h=weight in grams/10+200
This must
then be divided by the number of feeds in the day (6 or 5 according
to the age).
As soon
as solid foods are introduced , this must be considered when
calculating the total required.
·
Always prepare a little more than the
child will take ; this avoids involuntarily restricting the amount
taken; it is the child and its growth which ought to dictate the size
of the feeds.
N.B. : do
not keep the rest of the milk for the baby; give it to the older
children
6. 6.
Number of bottles:
·
At the beginning, the baby demands
frequent feeds but by 6 to 7 months feeds 4 times a day, as adults
do.
As with
the size of the feeds , it is the infant and its rate of growth
which determine their frequency.
Most
children are happy with 6 to 8 feeds a day from the first days of
life until they are 3 or 4 months old; they usually take 5 feeds a
day between 4 and 6 months , and after that change to 4 feeds day.
Exclusive milk feeding in early life is adequate for growth but after 4-6
months of age , mother’s milk is not enough for the infant’s
requirements . It is therefore, absolutely necessary from 6 months
or earlier that the infant has at least one non-milk feed each day.
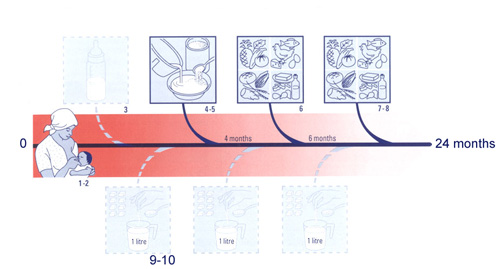
Fig.1-How to feed a young child properly .
The first more solid feed (gruel) should be offered at about 4 months:
this is known as supplementation and is usually well
tolerated. At about 5 or 6 months, a more varied diet (e.g.
vegetables ,meat ,fish, egg, cheese ,yoghurt) should be given; this
may be accepted reluctantly, even refused.
Refusal may be a normal expression of the infant’s personality. When this
happens, it is important to reassure the mother and to encourage her
to persist.
4
|
4
HOW TO FEED A CHILD PROPERLY (FIG.1) |
1.
Offer the breast from birth.
2.
Breast-feed for 24 months if possible , and
in any case until a complete and varied diet is accepted by
the child.
3.
Bottle-feeding is potentially dangerous for
all infants; whenever bottle feeding is necessary, make feeds up
very carefully , strictly obeying the rules of hygiene and
composition.
4.
Supplementary foods are not needed until 4
months of age . From then , or earlier if the weight curve falters,
a supplement (e.g. gruel) should be given with a spoon.
5.
Gruels should be cereal-based
and enriched with one or , preferably , several locally available
foodstuffs , rich in proteins and fats.
6.
From the age of 6 months, the infant
should have the following once or twice a day:
Infants should have at least 4 meals a day until the age of 5
years.
7.
From 6 months, infants should take part in
family meals , which should contain a variety of foods; spices
should not be given.
8.
Refusal to eat is very common in young
children . Check that the diet is well-balanced; have the child
weighed and carefully examined.
9.
Sick children need semi-liquid diets which
must be very nourishing and enriched with fresh fats and sugar.
10.
Children with diarrhoea should be kept on the
breast and given oral dehydration solution .
Meals should be nourishing , for example a mixture of curdled
milk , oil and sugar, which does not aggravate the diarrhoea . If
vomiting occurs , patiently persist with small quantities at a time
by spoon , without giving more than a small bowlful (150-200 g).
| 


