|
پروفسور محمد حسین سلطان زاده
استاد
دانشگاه علوم پزشکی شهید بهشتی
متخصص کودکان ونوزادان
طی دوره بالینی عفونی از میوکلینیک آمریکا
دبیر برگزاری کنفرانس های ماهیانه گروه اطفال
دانشگاه علوم پزشکی شهید بهشتی
|
دكتر مژگان هاشميه
فوق تخصص خون اطفال
دكتر رضا شياري
فوق تخصص روماتولوژي
اطفال
معرفي كيس:خانم دكتر مهسا مهري
رزيدنت بيمارستان
امام حسين
خانم دكتر سيما بهرامي
رزيدنت بيمارستان
مفيد
اقاي دكتر پيام سامعي
رزيدنت بيمارستان
شهدا
خانم دكتر لاله محمدي
رزيدنت بيمارستان
لقمان
دكتر عبدالله كريمي
فوق تخصص عفوني اطفال
دكتر محبوبه منصوري
فوق تخصص الرژي و
ايمونولوژي
دكتر تقي ارزانيان
فوق تخصص خون اطفال |
دكتر مژگان هاشميه
فوق تخصص خون اطفال

ÒFever
of Unknown Origin
Ò
Terminology
Ò
Fever > 38.3oC (101 oF) on several occasions.
Ò
Illness of more than 3 weeks’ duration.
Ò
Uncertain diagnosis after 1 week of study in the hospital.
Ò
Etiology
Ò
Infection 30-50%
Ò
Collagen vascular disease 10-20%
Ò
Neoplasms 5-10%
Ò
Miscellaneous 10-20%
Ò
No diagnosis 10-25%
Ò
Infectious Causes of FUO
Ò
Mononucleosis (EBV & CMV)
Ò
Systemic
viral syndrome
Ò
Urinary
tract infection
Ò
Intra-abnominal and Retroperitoneal Abscesses
Ò
Osteomyelitis
Ò
Respiratory tract infection
Ò
Tuberculosis
Ò
Bacterial
meningitis
Ò
Endocarditis
Ò
Enteric
infection
Ò
Malaria
Ò
HIV
infection
Ò
Non Infectious Cause FUO
Ò
Miscellaneous
Drugs and nutritional supplements
Pseudofever disorders
Pulmonary embolism
Hyperthyroidism
Kawasaki disease
Ò
EVALUATION OF OUR PATIENT
Ò
CBC=ß
thal minor
ESR=140
CRP=9.6
PBS(MALARIA&BORRELIA)=NEG
Ò
SGOT=40
SGPT=31
ALK.P=355
LDH=380
TG-CHOL-LDL-HDL=NL
Ò
C3=NL ,
C4=NL ,
CH50=NL
ANA=NL ,
C-ANCA&P-ANCA=NL
anti ds-DNA=negative
anti cardiolipin=negative
anti phospholipid=negative
R.F=negative
Ò
Blood
Culture: NEG
BACTEC: NEG
U.A: NL , U.C: NEG
CSF.A&CSF.C: NL
CSF(TB PCR-ADA-WRIGHT): NL
ASO.TITER: NL
FIBRINOGEN: NL
immunE electrophoresis: NL
Ò
BRUCELLA
SEROLOGY:NEG
IFA KALA AZAR:NEG
viral serology(hbv &hcv&HIV):NEG
Ò
BM
aspiration& biopsy:NL
BM flow cytometry:NL
CD25=NL
skin biopsy:
chronic lymphocytic vasculitis
Ò
sonography:mild splenomegaly+accesory spleen
spiral CT scan(chest and abdominopelvic):
mild splenomegaly
bone scan:NL
chest X-ray:NL
Ò
FMF Assay
ÒTEST
NO 1:
ÒThe
test is based on strip assay technique using genomic DNA. The assay covers
12mutions in the MEFV Gene as:
ÒE148Q,P369S,F479L,M680I(G/C),M680I(G/A),I692del,M694V,M694I,K695R,V726A,A744S,R761H.
ÒResult=Negative
ÒTEST
NO 2:
ÒThe
test is based on direct DNA sequencing for exon1,2,3,4,5,6,7,8,9,10 of the
Mediterranean fever gene.
ÒResult=
This individual has heterozygote mutation(R202Q) in exon2 of the MEFV gene
ÒFAMILIAL
MEDITERRANEAN FEVER
q
FMF
is an autosomal recessive disorder
q
characterized by brief acute, self-limited episodes of fever and polyserositis
that recur at irregular intervals
q
associated with development of amyloidosis.
Etiology
q
The gene responsible for FMF is mapped on 16p13.3. It is designated MEFV.
q
This gene
encoding a protein known as pyrin which is expressed in myeloid cells.
q
Exon 10 and exon 2 carry most FMF-associated mutations.
q
To date, more than 70 mutations have been discovered, mostly missense mutations.
q
The 5 most common mutations (M694V, V726A, M694I, M680I, E148Q) are found in
more than 2 ∕ 3 patients with FMF.
q
Approximately 70% of patients with clinical manifestations
of FMF are heterozygous
q
The most common missense mutation is M694V (substitution of methionine with
valine at codon 694)
q
occurs in 20-67% of cases
q
Associated with a greater disease severity and a higher incidence of
amyloidosis
q
It is also associated with increased risk for onset at an early age
Pathogenesis
q
The exact pathogenesis of the acute episodes of FMF is unknown.
q
Between episodes, patients with FMF have increased serum levels of interferon-γ
and enhanced production of other proinflammatory cytokines, such as TNF-α,
IL-1β,
IL-6, and IL-8, in circulating leukocytes.
q
Pyrin
acts as an anti-inflammatory factor by inhibiting processing of pro-IL-1
β
cytokine to the active form.
q
The defective (or mutated) pyrin found in patients with FMF is functionally
inactive.
q
As a consequence, stimulation of IL-1β
processing and secretion occur, resulting in increased IL-1β
levels that are responsible for the uncontrolled inflammation .
q
Another possibility that was previously more popular is C5a inhibitor
deficiency in patients with FMF.
q
C5a is a fragment of complement, an anaphylatoxin, and a potent chemotactic
agent .
q
The hypothesis is that a deficiency of C5a inhibitor, which is a consequence of
pyrin dysfunction in patients with FMF, allows further accumulation of C5a,
leading to the acute attack.
Clinical Manifestations
q
The onset of clinical manifestations occurs before 5 yr of age in
65% of cases and before 20 yr of age in 90% of cases.Onset
may be as early as 6 mo of age.
q
Exercise, emotional stress, infection, menses, and surgery may precipitate
acute episodes.
q
The typical acute episode lasts 1-4 days
q
includes fever and 1 or more symptoms of :
q
sterile peritonitis, manifested as abdominal pain (90%)
q
arthritis or arthralgia (85%)
q
pleuritis manifested by chest pain (20%)
Other manifestation:
a)
Erysipelas-like rash
b) myalgia
c) splenomegaly
d) scrotal
involvement
e) neurologic
involvement
f)
Henoch-Schonlein purpura
g)
hypothyroidism
Diagnosis
q
Genetic testing for the FMF gene confirms the diagnosis of FMF.
q
Genetics laboratories usually screen for only the 10 to 15 most common
mutations, and thus, rare mutations will be missed.
q
Therefore, the diagnosis of FMF is still based on clinical manifestations, with
genetic testing used as a confirmatory test .
Treatment
q
Attacks of FMF can be prevented by prophylactic
colchicine
(0.02-0.03 mg/kg/day; maximum 2 mg/day) .
q
65% of patients experience remission of
attacks
q
20-30%
experience improvement with significant reduction in the number and severity of
the episodes
q
5-10%
show no response.
q
Colchicine therapy decreases the probability of development of amyloidosis.
q
Poor compliance is common,owing to gastrointestinal side effects .
q
Toxic effects (acute myopathy and bone marrow
hypoplasia) can be seen with doses >0.1 mg/kg, resulting in lethality at a dose
≥0.8mg/kg.
It has also been shown that biologic treatments,
especially the IL-1 inhibitor anakinra, produce a
beneficial response in cases of FMF that do not respond to colchicine.
Complications and Prognosis
In 30-50% of untreated children and in 75% of adults with FMF, a form of renal
amyloidosis develops .
Renal disease manifests as proteinuria that progresses to nephrotic syndrome and
renal failure .Transplantation may be required for renal failure.
Mortality
Mortality from FMF usually results from complications of renal failure and
amyloidosis, such as infection, thromboembolism, and uremia.
دكتر رضا شياري
فوق تخصص روماتولوژي اطفال

معرفي كيس:خانم دكتر مهسا مهري
رزيدنت بيمارستان امام حسين

پاسخ:
تشخيص هاي افتراقي:
خانم دكتر سيما بهرامي
رزيدنت بيمارستان مفيد


�
معرفی یک مورد
تب طول کشیده
�
شکایت اصلی
(chief complaint):
تب طول کشیده به همراه ضایعات پوستی
�Present
illness:بیمار
دخـتر 8 سـاله ای اسـت که در تـاریخ 3 مـرداد 90 به عـلت تـب و ضایعات پـوستی
بستری گردید تب وی حدودا از 40 روز قبل آغاز شده و بجز علایم کوریزا در
ابتدای تب، نکته دیگری نداشته است . طی دو نوبت مراجعه سرپایی تحـت درمان با
کلیندامایسین و پنیسیلین قرار می گیرد، امـا تب وی همچنان ادامه می یابد. در طی
دومین هفته بیماری، بیمار دچار لرزهای تکان دهنده میشود و ضایعات پوستی ابتدا در
اندام فوقانی و سپس اندام تحتانی و باسن ایجاد می شود . وی جهـت بـررسی در
یـک مـرکز خصوصی بستری میشـود و در طی 18 روز بستری در آن مرکز تحت آزمایشات مختلف
قرار میگیرد که یافته های مهم درCBC
شامل
آنمی ، ترومبوسیتوپنی، بالا بودن
ESR,CRP
ودر
سونوگرافی وجود اسپلنومگالی خفیف بود.
�
وی در طـی
بسـتری در آن مرکـز تحـت درمان با کوتریموکسازول قرار گرفـت و به عـلت عـدم قطع تـب
داروهـای وی به سفتریـاکسون + وانـکومایسین تغییر یـافت و نهایتاً پالس
متیل پردنیزولون و
IVIG
دریافت کرد.به دنبال این درمان تب بیمار قطع میشود و بیمار با داروی استامینوفن
مرخص می شود به مدت 2 روز بـدون تب بوده اما راش پوستی هم چنـان وجود داشته است.
با شروع مجدد تب و با شک به بیماری لانگـرهانس هیستیوسیتوز، در بخش
اطفال
جهت بررسی بیشتر بستری می شود
�
در زمان بستری
حال عمومی بیمار خوب بود.
�
علایم
حیاتی:
38.6=
AT
درجه سانتی گراد
10.5/7BP=سانتی
مترجیوه
18=RR
در دقیقه
110=PR
در
دقیقه
�
در معاینه فیزیکی:
معاینه چشم
نرمال بود. معاینه
ENT
نرمال
بود. لنفادنوپاتی در هیچ قسمتی از بدن نداشت. معاینه قلب و ریه نرمال بود. معاینه
شکم نرمال و بدون ارگانومگالی بود. معاینه تناسلی نرمال بود. معاینه عصبی نرمال
بود. در پوست، راش اریزپل مانند، گرم، تندر، بدون خارش و پوسته ریزی با اندازه های
متفاوت و حد اکثر 4*3 در انتهای اندام تحتانی، شکم و باسن وجود داشت.
�
سابقه قبلی و
سلبقه فامیلی:
�
بیمار حاصل
زایمان طبیعی، بدون سابقه قبلی بیماری و بستـری است. والـدین منصوب نبوده،
مادر سابقه تالاسمی مینور دارد. فرزند دیگر پسر 12 سـاله و سالم است. سـابقه مسافرت
اخیر نمیدهد.
�
بعد از بستری
آزمـایشـات زیر جهت بیمار انجام شد که نتایج به این صورت میباشد:
Problem
list
�
Fever and shake
�
Erisiploid, painful and warm rash
�
Anemia
�
Thrombocytopenia
�
ESR
�
CRP
�
Skin biopsy chronic lymphocytic vasculitis
�
Splenomegaly
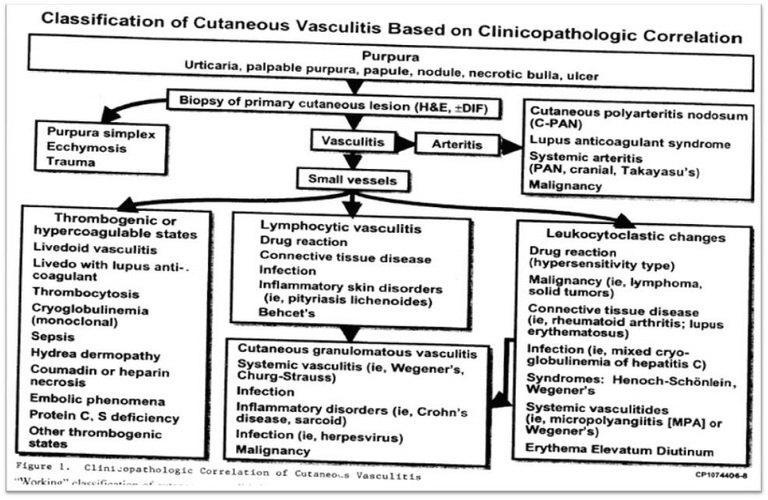
lymphocytic vasculitis
�
lymphocytic vasculitis is defined by necrotizing destruction of blood vessel in
the setting of lymphocytic inflammation in and around the vessel wall. It may
evolve over time into a granulomatous pattern.
Drug
reaction
�
Positive finding:
�
Skin lesion
�
Negative finding:
�
No
history about use of any drug before beginning of disease
Connective
tissue disease
�
SLE
SLE Is a chronic
autoimmune disease characterized by multi system inflammation and the presence
of circulating auto antibodies directed against self antigens.
�
Positive finding:
�
Fever
�
Cutaneous vasculitis
�
Thrombocytopenia
�
Anemia
�
Splenomegaly
SLE
�
Negative finding:
�
ANA
: negative
�
C3-
C4- CH50: NL
�
Anti dsDNA: NL
�
Anti phospholipid: NL
�
Anti CARdiolipin: NL
Behcet’s
�
Behcet’s
is an autoinflamatory multi system disorder originally described as recurrent
oral and genital ulceration associated with relapsing iritis or uveitis and is
often characterized by cutaneous, arthritic, neurologic, vascular,
gastrointestinal manifestations.
�
The
international study group criteria for diagnosis of Behcet’s
are oral ophthus that recur at least 3 times within 12 mo accompanied by 2 of
the following:
�
recurrent genital ulceration
�
Eye
lesions (anterior or posterior uveitis or retinal vasculitis
�
Skin lesion (erythema nodosum, pseudofuliculitis or acneiforme nodules
�
Positive pathergy test result.
�
Positive finding:
�
Skin lesion
�
Negative finding:
�
No
history of oral or genitalia ulcer
Infections
�
Herpes virus:
The hallmarks of
common HSV infections are skin vesicle and shallow ulcers. Lesions begin as
grouped erythematous papules that progress to vesicles. Pustules, ulcers and
crusts and then healing without scanning in results in multiple discrete lesions
and involves a larger surface area recurrences are sometimes associated with
local edema and lymphangitis or local neuralgia.
HSV
�
Positive finding:
�
------
�
Negative finding:
�
Type of skin lesions, no history about vesicle lesion
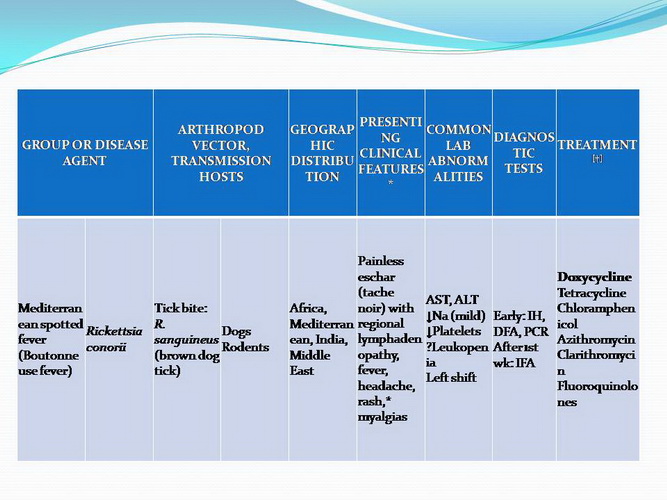
Ricketsial
infection
�
Rocky mountain spotted fever:
RMSF is the most
frequently identified and most severe rickettsial disease in the USA.
RMSF should be
considered in the deferential diagnosis of fever, headache and rash in the
summer months specially after tick exposure.
The illness is
initially non specific with symptoms including headache, anorexia myalgia,
restlessness pain and tenderness of calf muscle, GI symptom including nausea,
vomiting, diarrhea, abdominal pain occur commonly early in the disease.
Rash usually
appear only after 2 -4 days of illness.
Other symptoms
including central nervous system infection, pulmonary disease,
hepatosplenomegaly.
confirm RMSF
actually must be based on compatible epidemiologic, clinical and laboratory
features.
Definitive
diagnosis is most often accomplished by serology. The gold standard for
diagnosis is a 4
–
fold increased in IgG antibody titer (IFA)
RMSF
�
Positive finding:
�
Fever
�
Rash
�
Splenomegaly
�
Negative finding:
�
IFA:
negative
Mediterranean spotted fever
Typical finding
include fever, headache, myalgia and macula popular rash that appears 3-5 days
after onset of fever
Diagnosis of MSF
is the same as that for RMSF.
MSF
�
Positive finding:
�
Fever
�
Rash
�
Negative finding:
�
IFA:
negative
Typhus
group rickettsioses
�
Murine typhus
The incubation
period varies from 1-2 w
Symptoms
including rash, myalgia, vomiting, cough, headache and diarrhea or abdominal
pain, hepato splenomegally and lymphadenopathy are reported often among children
Murine
typhus
Diagnosis must be
based on clinical suspicion. Confirmation of the diagnosis is usually
accomplished by comparing acute and convalescent phase antibody titer obtained
with the IFA.
Murine
typhus
�
Positive finding:
�
Fever
�
Rash
�
Splenomegaly
�
Negative finding:
�
IFA:
negative
granulomatous vasculitis
�
ANCA-
associated vasculitis
�
Wegner
WG occurs at all
ages and targets the respiratory tract and the kidneys
WG occur in
adults. It does develop in children with a mean age at diagnosis of 14 yr.
There is a female
predominance.
The diagnosis is
confirmed by the presence of anti -PR3-specific ANCA and the finding of
necrotizing granulomatous vasculitis on pulmonary- sinus or renal biopsy.
Wegner
The ANCA test
result is positive in 90% of children with WG.
�
Positive finding:
�
Fever
�
Skin vasculitis
�
Negative finding:
�
C-
ANCA&P-ANCA: NL
CCS
The presence of
choronic asthma and pripheral eosinophilia suggested the diagnosis of CSS.
In 70% of cases
of CSS mpo- ANCA are more common than PR3 ANCA.
Inflammatory disorder
�
Crohn’s
disease:
Choronic
Inflammatory disorder of the bowel involves any region of the alimentary tract
from the mouth to the anus.
Extra intestinal
manifestation oral aphthous ulcers, pripheral arthritis, erythema nodosum
digital clubing, episcleritis, renal stones and gall stones.
Inflammatory disorder
The diagnosis of
Crohn depends on finding typical clinical features of disorder (history,
physical exam, laboratory study and endoscopic or radiologic finding).
Crohn
�
Positive finding:
�
Skin lesion
�
Negative finding:
�
No
history about GI problem
Sarcoidosis
This Is a rare
multi system granulomatous disease of unknown etiology.
Children may
present with non specific symptoms such as fever, weight loss and general
malaise.
In older children
pulmonary involvement is most frequent consist of dry, persistent cough.
Sarcoidosis
Extra thoracic
lymphadenopathy and infiltration of the liver, spleen and bone marrow also occur
often.
Cutaneous disease
such as plaques nodules, erythema nodosume.
Other
manifestation consists of ocular involvement, central nervous system, kidney
disease, heart symptoms.
Sarcoidosis
Early onset
Sarcoidosis in older children is triad uveitis, arthritis and rash.
Diagnosis
requires characteristic non caseating granulomatous lesions in a biopsy
specimen.
Sarcoidosis
�
Positive finding:
�
Skin lesion
�
Fever
�
splenomegaly
�
Negative finding:
�
Skin biopsy
HLH
The diagnosis of
HLH is established by full filing 1 or 2 of the following criteria:
�
A
molecular diagnosis consistent with HLH (PRF mutation, SAP mutation).
�
Having 5 out of 8 of the following.
�
Fever
�
Splenomegaly
�
Cytopenia (affecting >= 2 cell lineages, Hb<=9 (or <=10 for infants<=4 W of
age), PLT<100000, NUT<1000)
HLH
�
TG>=265 and or hypofibrinogenemia<=150 mg/dl
�
Hemophagocytosis in the bone marrow, spleen or lymphnode with out evidence of
malignancy
�
Low
or absent NK cell cytotoxicity
�
Hyper ferritinemia>= 500
�
Elevated soluble CD 25
HLH
�
Positive finding:
�
Fever
�
Anemia
�
Thrombocytopenia
�
Splenomegaly
�
Negative finding:
�
Fibrinogen: NL
�
BMA,
BMB: NL
�
CD
25: NL
�
TG:
NL
اقاي دكتر پيام سامعي
رزيدنت بيمارستان شهدا

به نام خدا
شرح حال:
دختر 8 ساله با تب از 40 روز قبل
عدم
پاسخ به درمان آنتی بيوتيکی
(کليندامايسين، پنی سيلين،کوتريماکسازول،سفترياکسون، ونکومايسين)
شروع ضايعات پوستی از هفته دوم
اسپلنومگالی خفيف
IVIGپاسخ
موقت تب به درمان کورتيکواستروييد و
ادامه وجود راشها و بازگشت تب
نکات مثبت پرونده:
تب
راش
گرم ، تندر، بدون خارش ، بدون پوسته ريزی
اسپلنومگالی خفیف
)ESR=140
خيلی بالا (ESR
واسکوليت لنفوسيتيک مزمن در بيوپسی
نکات مبهم پرونده:
انجام شده؟PPD
اکوی قلب ؟
سابقه برخورد با حيوانات؟
الگوی تب؟
علل تب طول کشيده همراه راش:
عفونتها
بيماريهای روماتولوژيک (بافت همبند و اتوايميون)
بيماريهای نئوپلاستيک
تب
دارويی
تب
ساختگی
عفونتها :
1- باکتريال
الف:
بروسلا
+ :
تب
+ :
اسپلنومگالی
- :
کشت خون منفی
(باید
تکرار شود)Grey
Zone-
: سرولوژی :
TB
ب.
؟ PPD
سابقه تماس؟
نرمالCXR
علائم تنفسی ندارد
ج .
اندوکارديت
اکوی قلب ؟
-
: کشت خون منفی
-
: عدم وجود تظاهرات بالینی نظیر:
Osler nodes
،
splinter
hemorrhages
،Janeway
lesions
-
: بيمار بدحال نمی باشد
د.
عفونتهای ریکتزيايی
Mediterranean spotted fever
(Rickettsia
conorrii)
برخورد با سگ ؟
-
: عدم لنفادنوپاتی
Qه.
تب
(C. burnetii)
عامل کوکسيلا بورنتی
انتقال : بيشتر از طريق آئروسل عفونی
+ :
تب همراه آزمايشات نرمال
کمتر از 20 (در 80% موارد)ESR
- :
معمولا
- :
هيپرفيبرينوژنمی (در 67% موارد)
مثبت (در 50% موارد)RF
- :
2-
عفونتهای ويرال:
)
با سرولوژی رد شده.HIV
و
HCV
و
HBV(
EBV
-
CMV
-
3-
قارچها
- هیستوپلاسموزيس
تب
دارويی
معمولا 72 ساعت بعد از قطع دارو بهبود می يابد.
تب
ساختگی
با
بستری در بيمارستان و ثبت الگوی تب رد می شود
:اختلالات
نئوپلاستيک
نرمال، بيوپسی و آسپيراسيون مغز استخوان نرمال،LDH
نرمال،
CBC
نرمال : احتمال ضعيفCT
نرمال،
Bone Scan
اختلالات روماتولوژيک :
-
: علائم آرتريت يا آرترالژی ندارد
-
: معاينه چشم نرمال است
-
: آزمايشات نرمال است
C3, C4, CH50,
ANA, C-ANCA, P-ANCA, RF
Anti ds-DNA, Anti
Cardiolipin, Anti Phosphlipid
FEATURES
THAT SUGGEST A VASCULITIC SYNDROME
CLINICAL FEATURES
�
Fever, weight loss, fatigue of unknown origin
�
Skin lesions (palpable purpura, vasculitic urticaria, livedo
reticularis, nodules, ulcers)
�
Neurologic lesions (headache, mononeuritis multiplex, focal central nervous
system lesions)
�
Arthralgia or arthritis, myalgia, or myositis
Serositis
�
Hypertension
�
Pulmonary infiltrates or hemorrhage
LABORATORY
FEATURES
�
Increased erythrocytes sedimentation rate or C-reactive protein level
�
Leukocytosis, anemia
�
Eosinophilia
�
Antineutrophil cytoplasmic antibodies
�
Elevated factor VIII–related antigen (von Willebrand factor)
�
Cryoglobulins
�
Circulating immune complexes
�
Hematuria, proteinuria, elevated serum creatinine
�
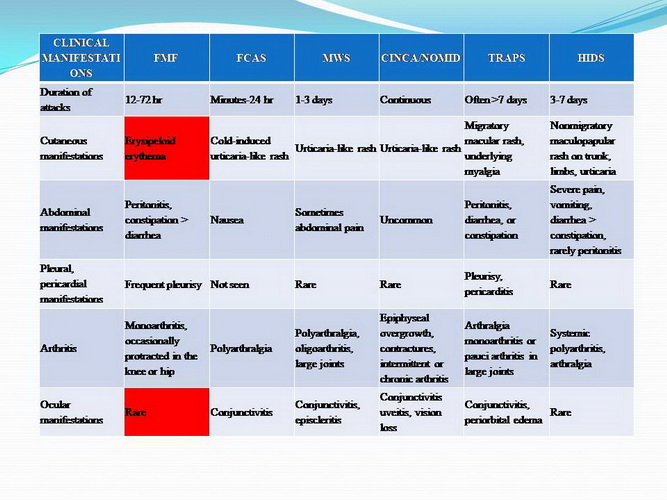
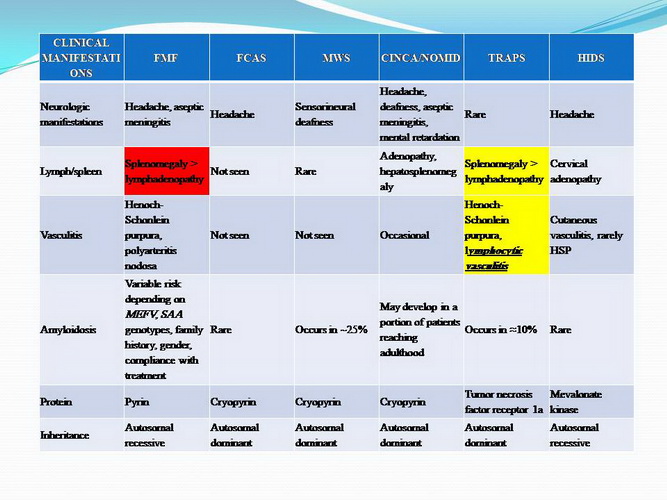
HEREDITARY PERIODIC FEVERS:
�
FMF (Familial
Mediterranean Fever)
�
TRAPS ( TNF
Recptor Associated Periodic Syndrom)
�
HIDS ( Hyper Immunoglobulinemia D Syndrom)
�
MWS
(Muckle Wells Syndrom)
�
FCAS (Familial Cold Autoinflammatory Syndrom)
�
PFAPA (Periodic Fever ,Aphtous stomitis, Pharyngitis , and cervical
Adenitis)
:
FMF
بيماری نمی شود.
ممکن است از موتاسيونهای غیرشايع باشدبررسی ژنتيک باعث رد.
:
TRAPS
بيوپسی پوست به نفع می باشد.
خانم دكتر لاله محمدي
رزيدنت بيمارستان لقمان


IN THE NAME OF
THE ABSOLUTE LIGHT
Problem List
1-Prolonged Fever
2-Skin Lesion
3-Skin Biopsy:Chronic Lymphocytic Vasculitis
4-Anemia,Trombocythopenia,Elevated ESR & CRP
5-Mild Splenomegaly
6-chills
Erythema Nodosum
Streptococcus Pharyngitis
EBV
Sarcoidosis
TB
Hodgkin lymphoma
HIV
Histoplasmosis
Cat Scratch Disease
leptospirosis
Yersinosis
FUO
1-Generalized :
TB
Sarcoidosis
Cat Scratch Disease
Leptospirosis
Malaria
Salmonellosis
Yersinia
Tularemia
HIV
Trench Fever
Brucellosis
2-localized Infection:
Bone & Joint
Infective Endocarditis
Intra Abdominal Abscess
Hepatic Infection
Upper Respiratory Tract Infection
UTI
3-Connective Tissue:
Vasculitis
4-Neoplasm:
Lukemia
lymphoma
5-Other Causes:
Periodic Fever:
1- FMF
2-TRAPS
3-HILLS
4-Cyclic Neutropenia
IBD
Immune Deficiency
Fctitious Fever
Drug Fever
Definitive DDX
TRAPS
FMF
EBV
SLE
THANKS FOR YOUR ATTENTION
دكتر
عبدالله كريمي
فوق تخصص عفوني اطفال


دكتر محبوبه منصوري
فوق تخصص الرژي و ايمونولوژي


دكتر تقي ارزانيان
فوق تخصص خون اطفال




















