|
پروفسور محمد حسین سلطان زاده
استاد
دانشگاه علوم پزشکی شهید بهشتی
متخصص کودکان ونوزادان
طی دوره بالینی عفونی از میوکلینیک آمریکا
دبیر برگزاری کنفرانس های ماهیانه گروه اطفال
دانشگاه علوم پزشکی شهید بهشتی
|
آقای
دکتر سعید صدر
فوق تخصص ریه اطفال
به اتفاق اعضای هیئت
علمی بیمارستان کودکان مفید
|
معرفي بيمار
History:
A girl with 11 years old was
admitted to pulmonology ward with dyspnea, orthopnea, periorbital and
extremities edema and hepatomegaly.
During last 3 months she was
suffered from dyspnea on exertion, cyanosis during sleep and sometimes edema in
extremities.
She was visited by physician several
times and admitted and different lab test was performed.
Prior to admission in our hospital
she was treated as asthma with bronchodilators, Inhaler corticosteroid (ICS) and
prednisolone for 2 months.
Past Medical History:
At
birth: (BW=3.5 kg , NVD, no respiratory distress)
She had
signs of weakness from 3 years of age such as weakness in standing from sitting
position.
She had
dyspnea on exertion from 7 years of age.
Family history:
Her
brother has weakness, especially the transition from supine to sitting.
Recently he developed breathlessness and cyanosis during sleep.
History
of death in infancy in sibling with respiratory distress.
History
of weakness and respiratory problems and death in second degree relatives.
Parents
are relative.
Physical Examination:
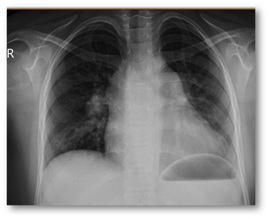
General
appearance: ill, pallor, Respiratory distress
Vital
sign: RR: 35/min, BP: 95/50 mmHg, T: 37, HR: 160/min, SpO2
at room air: 82%
Weight:
33 Kg
Rapid
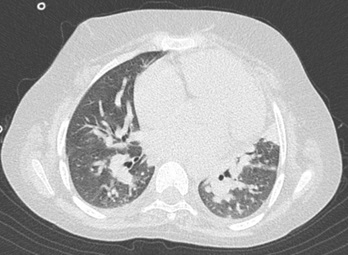
shallow breathing, Inspiratory fine crackles in base of lungs
Hepatomegaly
Pitting
edema in extremity
Weakness
( upper and lower extremity: 3/5), Decreased DTR
Others:
Normal
Laboratory tests:
CBC-Diff, BS, Na, K, BUN, Cr,
Ca, Ph, ALT, ALK-Ph: Normal
AST: 50 LDH: 710 CPK:
260 Aldolase: elevate
Thyroid Function Test: Normal
ABG: (PH: 7.38 PCO2:
65 mmHg HCO3:35 PO2: 55 mmHg )
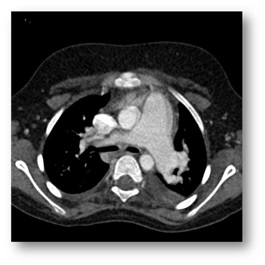
Cardiology consult: ECG: RVH, Echocardiography: RVH, Pulmonary
Atrial Pressure= 70 mmHg
Disease process:
She was admitted to pulmonology
ward: treatment for Pulmonary Atrial Hypertension (PAH) and right heart failure
was started.
After 3 days of admission she
developed gasping respiration, decreased Sao2 and raised PCO2
( PCO2=90mmHg) during
sleep and undergone intubation and mechanical ventilation.
6 days after intubation, patient was
extubated and undergone non-invasive ventilation (NIV).
8 days after start of NIV, she was
discharged with NIV.
Other diagnostic studies were
performed.
تشخيص شما چيست؟



