|
پروفسور محمد
حسین سلطان زاده
استاد دانشگاه علوم پزشکی شهید بهشتی
متخصص کودکان ونوزادان
طی دوره بالینی عفونی از میوکلینیک آمریکا
دبیر برگزاری کنفرانس های ماهیانه گروه اطفال
دانشگاه علوم پزشکی شهید بهشتی
|
معرفی : دکترمحمد رضا علائی
فوق تخصص غدد اطفال
به اتفاق اعضای هیئت علمی گروه کودکان
بیمارستان لقمان حکیم
|
تشخیص
Familial chylomicronemia syndrom
TG = 24000
CHOL = 1600
Lipoprotein electrophoresis :
chyl = 40% ( 0 % )
LDL = 41% (40-60%)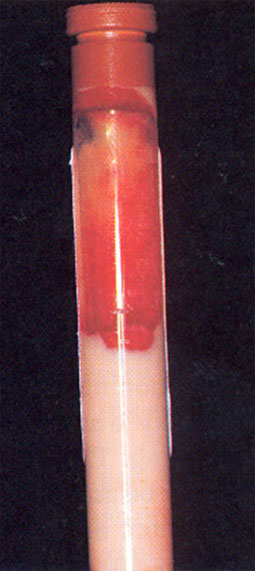
VLDL = 15% (15-25%)
HDL = 4% (25-35%)
Disorders of lipoprotein metabolism
Children with elevated chol Level should be identified early in life to try to
reduce the associated risk of heart dis.
Adult cardiovascular dis has its roots in childhood
Hyper chol. : > 75th percentile for the age & sex
Hyper TG >95TH percentile for age & sex
Hyper TG is also a risk factor for premature CHD , the risk is less well defined
than hyper CHOL.
Primary prevention of CHD is important
Plasma lipoprotein metabolism & transport
Plasma lipid & lipoprotein levels
During the first few month of life , chol increase largely Because of changes
in LDL.
HDL CHOL are compatible in M & F early in life but decline markedly in M during
the 2th decade
TG rise transiently in M & F in the first year ,fall to a mean 50-60 in the few
years & then rise by age 20yr.
Screening for hyper CHOL.
Parental CHOL > 240 mg/dl
Children with incomplete or un available FHX.
Other risk factors for CHD ( obesity ,cigarette smoking , HTN, DM, inactivity,
low HDL)
Total chol < 170 mg/dl : re-evaluated in 5yr
Total CHOL > 200mg/dl : fasting lipid profile
Total CHOL 170-199 MG/DL : another CHOL measurement
positive FHx Of Premature coronary heart dis. : lipid profile
Lipid profile ( total & HDL CHOL, calculated LDL CHOL ) after a 12 hr fast
LDL CHOL= total chol – [HDL+ ( TG/5)]
Treatment of hyperlipidemia
Dietary management
For child with average LDL CHOL > 110 mg/dl older than 2yr is the best initial
Intervention
Step 1 diet :
fat < 30% total cal. < 100 mg chol/1000 cal ( max 300 mg/24hr)
Minimal goal : LDL< 130 , ideal goal: LDL<110
Step 2 in diet :
Fat < 20% total cal. < 7% calories as saturated fat , < 66 mg chol /1000cal (
max 200 mg/24hr)
Response to dietary management : variable & < 10-15%
Children < 2yr require a relatively large amount of cal maintain their rapid
growth
Total caloric content
Wt loss in overweight individuals
Adverse effect in extreme dietary changes ( ↓ essential nutrients - electrolyte
abnormalities , orthostatic dizziness, GE discomfort , headache, cold
intolerance , menstural irregularities, peripheral neuropathy)
Sudden cardiac death
Yo-yo dieting
Nutritional composition
↑ intake vegetable fruits cereals & other complex carbohydrate sources
Saturated fat : ↑ total Cho& LDL ,↓ HDL
Polyunsaturated fat : ↓LDL, HDL↓
Monounsaturated fat :↓LDL, NLor↑ HDL
Soluble dietary fiber : ↓VLDL ,↓ LDL
Dietary supplement
Plant sterols ( 2 gr daily) : ↓LDL ( 10 to 13 % )
Fish oils : ↓ TG & anti PLT benefits
Physical activity
Regular physical activity
Moderate physical activity( expand a minimum of 200 kcal/day)
Improve lipoprotein profiles
Long term is most effective
30 to 60 minutes for 4 to 6 times/week
Walking, swimming, bicycling , jogging
Drug therapy
Child >= 10yr after a adequate trial of diet therapy :
LDL remains > 190 mg/dl
LDL > 160 mg/dl &
positive FHX of premature CHD
Two or more other risk factors ( DM ,HTN , smoking, low HDL, sever obesity ,
physical inactivity )
Secondary hyper lipidemia
Most of the hyper TG & hyper chol is secondary to exogenous factors or
underlying clinical disorders
Obesity , hypothyroidism , DM, nephrotic synd. ,renal failure, GSD, tay sachs,
niemanpick, congenital biliary atresie , SLE
Thiazid diuretics , steroid , beta drenergic blocking agent , immunosuppressants
Primary ( genetic) dyslipidemia
frederickson classification
Disorder associated with hyperchol. & severely elevated TG ( > 1000 mg/dl )
Fasting TG > 1000 mg/dl in children reflect sever hyperchylomicronemia &
indicate an underlying genetic disorder
The major clinical compilication is acute pancretitis
Familial chylomicronemia synd.
AR
LPL or apoc-2 deficiency ,Approximately 1/1 million person
May be evident as early as 2 days
May be silent & discovered incidentally ( lactescent blood)
The most common clinical presentation is acute , recurrent episodes of abdominal
pain
The age quite variable
Pains may be vary from mild infantile colic to severe peritonitis
Generalized or localized
Spasm , rigidity or rebound tenderness
Fever or leukocytosis → surgical intervention (usually a milky exudate un the
peritoneal cavity is the only finding)
Anorexia
Abd. Tenderness
Vomiting
Diarrhea
acute panceratitis
Well recognized complication
Sever abdominal pain
Hypotension
Sweating
Shock
Pancreatic necrosis without calcification
The serum amylase level may be very high or normal
TG > 1000 mg/dl
Infants & children with recurrent abdominal pain & pancreatitis & familial
pancreatitis should be examined for hyper chylomicronemia
Hepatosplenomegaly
Ingestion chylo by the RE SYSTEM
Particularly prominent in infants & children
Decrease of size within 24 to 48 hrs of initiation of the fat free diet
Sometimes pain due to splenomegaly
Fat embolism
Seizure , transient paralysis
GI bleeding
Cutaneous eruptive xanthoma
In about 50% of pts
On the buttoks ,back,proximal of the extremities and extensor surfaces
Yellow or yellow center
1-5 mm in diameter
Neither painful nor pruritic
TG >2000
Complete disappearance may take as long as 3 wk
Lipemia retinalis
Characteristic of long standing hyperlipidemia
Whitish or pinkish discoloration
Rarely wite diposits of lipid in retina
micro aneurysm & hemorrhages
Intermittent swelling of the scrotum
Milky effusion in tunica vaginalis
Swelling & mottling of the legs
Anemia , leukopenia & persistent thrombocytopenia
The very high lipid produce artefactual lowering of the values of many solutes
The degree of error is approximately 1% for each 0.9% gr/dl TG
Do not have hyperuricemia & abnormal GLU. Tolerance
Diagnosis
Based on the clinical presentation & some key lab features
Plasma is lactescent
TG> 1000 mg/dl may be as high as 15000 mg/dl
Total CHOL levels are elevated
CHOL/TG ratio always less than 0.2 & often less than 0.1
Refrigerator test ( 18-24 hr at 4 c) : cake of chylomicrons forms on the surface
& inferanatal layer is clear
Lipoprotein electerophoresis : marked elevated chylo.
DX. Can be confirmed by quantitation LPL activity in plasma after IV heparin
injected
LPL activity of about 50% of normal in parents
Heterozygote may have hyper TG but fasting levels of TG are usually NL or near
NL
TREATMENT
Restriction of total dietary fat
Most recommendations : TG < 1000 or even < 750 mg/dl
There is no specific problem with saturated or unsaturated fat
Total fat < 15% or 10% of daily calories
0.5 gr/kg useful in initiating therapy in children
caloric supplementation with medium-chain TG can be useful
No single meal should contain more than 20 gr of fat
Management is very difficult & TG may rise suddenly from a few hundred to
several thousand mg/dl following a single fat filled meal
If necessary , TG lowering medications (niacin or fibrates or fish oil) may be
added
FFP in APOC -2 deficiency
Type V hyperlipoproteinemia (HPL)
Common in adult
DX. With TG>1000 mg/dl without LPL or apoc- 2 deficiency
Acute pancreatitis
Positive FHX. Of hyper TG
DM or GLU. Intolerance
Nephrotic synd
Esterogen therapy , heavy alcohol use
Discontinue of drugs that exacerbate hypre TG
Control of underlying dis.
Dietary management
regular aerobic exercise
Drug therapy




