|
پروفسور محمد
حسین سلطان زاده
استاد دانشگاه علوم پزشکی شهید بهشتی
متخصص کودکان ونوزادان
طی دوره بالینی عفونی از میوکلینیک آمریکا
دبیر برگزاری کنفرانس های ماهیانه گروه اطفال
دانشگاه علوم پزشکی شهید بهشتی
|
دکتر مصطفی شریفیان
دکتر دلیرانی
فوق تخصص کلیه اطفال
با همراهی گروه متخصصین
بخش عفونی و تحقیقاتی بیمارستان
کودکان مفید |
تشخیص
Hemolytic-Uremic Syndrome
§
Hemolytic microangiopathic anemia:
§
Thrombocytopenia
§
Uremia: acute renal failure
§
Further symptoms / complications:
n
Central nervous system (seizures, hemorrhages)
n
Hypertension and heart failure
n
Liver / Pancreas (with diabetes mellitus)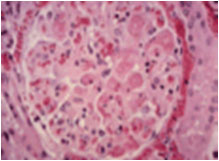
n
Eye: retinal bleedings
n
HUS: D+ and D-
n
D+ = Diarrhea-positive
n
Verotoxin (or Shigatoxin)-producing E. Coli
n
Other bacteria, e.g. Shigella....
n
Hemorrhagic colitis: mild – severe, intussusception
n
D- = Diarrhea-negative
n
Pneumococcal infections
n
Inherited and/or recurrent forms: e.g. complement (factor I/H) or vWF-cleavage protease deficiency
n
Others: Pregnancy, drugs …
n
„ Many“ cases of unknown cause
n
What is Post-Diarrheal Hemolytic Uremic Syndrome (D+HUS) and where did it come
from ?
n
The syndrome includes:
n
Acute kidney failure
n
Hemolytic anemia
n
Thrombocytopenia (low platelet count)
n
Most common cause of acute renal (kidney) failure in young children; also occurs
in older children and adults
Major Causes of TTP-HUS
n
Idiopathic: 37%
n
Drug-Associated: 13%
n
Cyclosporine
n
Tacrolimus
n
Mitomycin C
n
Bleomycin and cisplatin
n
Quinine
n
Autoimmune Disease: 13%
n
Scleroderma
n
SLE
§
Familial(AR-AD)
n
Infection: 9%
n
Viral(HIV,EBV,…)
n
Streptococcus pneumoniae
n
Bloody Diarrhea Prodrome: 6%
n
Shiga toxin production (ex: E. coli 0157:H7)
n
Shigella dysenteriae type 1
n
Pregnancy/Postpartum: 7%
n
Hematopoietic cell transplantation: 4%
Classic Symptoms of
TTP-HUS
n
Microangiopathic hemolytic anemia (MAHA)
n
Thrombocytopenia
n
Acute renal insufficiency (more common in HUS)
n
Neurologic abnormalities (more common in TTP)
n
Fever
Signs and Symptoms
n
Diarrhea (usually bloody) with severe pain; Dehydration
n
Pallor
n
Bruises,petechiae
n
Seizures and/or coma (occasionally)
n
Little (oliguria) or no (anuria) urine
n
High blood pressure ,edema
n
Pancreatic damage (diabetes)
n
Hepatosplenomegaly
n
Irritability,weakness,lethargy
Pathogenic Cascade;
from diarrhea to dialysis
n
Chain of events:
n
ingestion of Stx producing E. coli
n
multiplication in bowel
n
absorption of Stx into circulation
pathogenic cascade, cont.
n
Chain of events, cont.:
n
attachment of Stx to receptors in kidney, and occasionally other organs
n
movement of toxin into cells
n
cell injury or death
pathogenic cascade, cont.
the end result is:
n
hemorrhagic colitis (bloody diarrhea)
n
kidney injury, causing acute renal failure
n
damage of red blood cells causing anemia
n
trapping and destruction of platelets causing bleeding
n
occasional damage to other organs (brain, pancreas, heart, lungs, eyes)
Labs to Look For
n
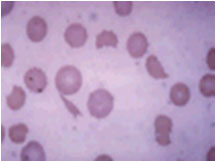
Schistocytes,helmet cells,burr cells,fragmented RBC on peripheral smear
n
Elevated LDH,Retic count and leukocytosis
n
Decreased Haptoglobin
n
Increased Creatinine
n
Thrombocytopenia
n
Hb level(5-9g/dl)
n
Coombs test (neg.),PT and PTT(normal)
n
Urinalysis (microscopic hematuria and proteinuria)
n
Differential Diagnosis of Thrombotic Microangiopathy:
n
Typical HUS (Shiga/vero toxin-related or rarely Strep. pneumoniae)
n
TTP (ADAMTS13 primary deficiency or inhibitor)
n
Atypical HUS (mostly complement-mediated)
n
Others: defective inborn errors of cobalamine metabolism, quinine-induced, other
drugs, HIV, malignancy, pregnancy/pre-eclampsia, SLE, scleroderma crisis and antiphospholipid antibody syndrome.
T.S. Jokiranta et al. Molecular Immunology 44 (2007). 3889-3900.
Treatment
n
Supportive care
n
Attention to salt and water balance
n
Dialysis for kidney failure
n
Blood transfusions for anemia
n
Platelet transfusions for bleeding
n
Aggressive nutritional support [TPN]
n
Treatment of high blood pressure
n
Treatment of seizures
n
Shiga toxin-binding resin ?
n
Plasmapheresis ?
n
FFP ?
n
Plasma Exchange
n
Initially performed daily until platelet count normalizes and hemolysis i mproved
n
Average of 7-16 daily exchanges needed
If Plasma Exhange Does not Work
(occurs in 10-20% of patients)
n
Increase to twice daily Plasma Exchange
n
Rituximab +/- cyclophosphamide
n
Vincristine
n
Intravenous immune globulin
n
Cyclosporine (* can cause TTP *)
HUS: Indications for dialysis
modality since 1995 (1)
n
Peritoneal dialysis:
„in general“ first choice
n
On ICU: CAPD
n
On ward: mainly automated PD
n
Hemodialysis
if
n
„older“ patient in „good general condition“ not requiring care in intensive care
unit
n
D-HUS and plasma-exchange (PEX) anticipated
n
life-threatening hyperkalemia
HUS: Indications for dialysis
modality since 1995 (2)
n
Continuous veno-venous hemo(dia)filtration
if
n
„in bad general condition“ (+/- PEX)
n
severe colitis
n
Plasma-exchange (PEX) or plasma infusion
if
n
D-HUS and inherited type / complement deficiency suspected
D- or D+ HUS with severe central nervous
system symptoms, e.g. impaired consciousness, neurological deficit
Acute PD
n
before 1995:
n
„stiff“ Cook-catheter or
n
„soft“catheter, inserted with trocar or
n
Tenckhoff
n
since 1995:
n
only Tenckhoff catheter
n
surgically placed by the surgeon (and the
nephrologist also in theatre) under general
anasthetic; at the same time insertion of
central venous line
Acute and chronic PD
n
Tenckhoff catheter:
HUS: clinical complications (1)
n
Hypertension: requiring medication

n
Cardiomyopathy:
n
Pancreatitis: Amylase ↑
n
Hepatopathy: Transaminases ↑
HUS: clinical complications (2)
n
Gastrointestinal tract: n = 4 (all D+)
n
2 intussusception
n
1 rectum perforation
n
1 severe colitis
n
Severe central nervous system: n = 7
n
4 D+: 3: remission,
n
3 D-: 2: sequelae (pneumococcal meningitis,
massive hemorrhage), (SLE)
n
Retinal bleeding: n = 2 (all D+)
Prognosis of HUS
n
With HUS caused by E. Coli O157:H7:
n
Mortality occurs in up to 3-5% of patients.
n
20% will develop CKD leading to ESRD.
n
With HUS associated with S. dysenteriae:
n
Mortality is greater, approaching 7%.
n
40% develop CKD.
n
With non-diarrhea associated HUS:
n
Mortality up to 25% in acute illness.
n
Up to 50% will require continued RRT.
Outcomes
n
Death in 3-5%, due to:
n
Brain damage (stroke and/or brain swelling)
n
Bowel necrosis and perforation
n
Heart damage
n
Lung injury
n
Multiorgan injury (seen in most fatal cases)
outcomes, cont.
n
Those who survive may be left with:
n
permanent kidney damage
n
brain damage
n
hypertension
n
diabetes
Monitoring
n
Chronic kidney failure may occur decades later (due to hyperfiltration injury)
n
most common in those who had prolonged kidney failure (oligoanuria) >10 days
n
proteinurea (protein in the urine) is an early sign
monitoring, cont.
n
Hypertension may begin years later (in those with chronic kidney damage)
n
Diabetes can latter occur (in those with pancreatic injury)
Conclusions (1): HUS
n
Incidence:
n
D+ >>> D- (over the last 35 years)
n
80% require dialysis
n
Outcome: D+ >> D-
n
Patient survival
n
Recovery of renal function
Conclusions (2): HUS – PD
n
Surgically placed Tenckhoff-catheter:
n
Simple technique
n
High efficacy
n
Low frequency of side effects / complications
n
PD in HUS is
n
safe
n
efficient
n
convenient
n
economic
Summary
n
D+ HUS is a life threatening complication of Stx producing E. coli and shigella,…
n
It occurs primarily in infants and young children, but also affects adults
n
Is fatal 3-5% of victims
n
Survivors (30-50%) are left with chronic kidney damage that can be progressive later in life
n
Life long monitoring is necessary




