|
پروفسور محمد
حسین سلطان زاده
استاد دانشگاه علوم پزشکی شهید بهشتی
متخصص کودکان ونوزادان
طی دوره بالینی عفونی از میوکلینیک آمریکا
دبیر برگزاری کنفرانس های ماهیانه گروه اطفال
دانشگاه علوم پزشکی شهید بهشتی
|
معرفی : دکتر
شاداب صالح پور
فوق تخصص غدد اطفال
به اتفاق اعضای هیئت علمی گروه کودکان
بیمارستان مفید
|
Case Presentation:
A nine year old girl with hepatosplenomegaly and thigh pain
The patient had been well until three years earlier, when she
began to have frequent episodes of epistaxis. Two years before
admission, mild abdominal distention developed. Periodic examinations
by her physician were reported to have revealed no abnormalities. Two
months before admission, the abdominal distention worsened but was
not accompanied by abdominal pain. Physical examination revealed
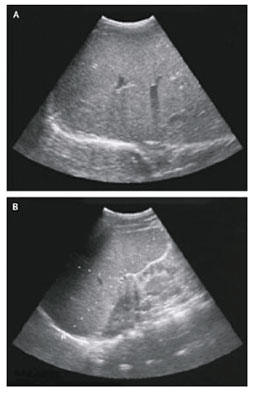
hepatosplenomegaly. An abdominal ultrasonographic study confirmed the
presence of hepatosplenomegaly, without evidence of portal-vein
thrombosis. The results of liver-function tests were normal or nearly
so, and tests for viral hepatitis A, B, and C were negative. Three
days before admission, pain developed in the right thigh, and on the
following day the patient was unable to walk because of pain. She was
admitted to the hospital.
She resided with her parents and three siblings, who ranged in age
from 14 to 17 years. She used no medications. She recalled having had
pain in the right leg about one year earlier; it had resolved
spontaneously. There was no history of previous hospital admissions,
sickle cell disease, recent travel, trauma, fever, night sweats,
anorexia, weight loss, jaundice, hematemesis, vomiting, diarrhea,
cough, arthralgia, easy bruisability, or bleeding gums, and there was
no family history of bleeding disorders, hemoglobinopathy, hepatic
disease, inflammatory bowel disease, autoimmune disease, or thyroid
disease.
The temperature was 38.6°C, the pulse 93 beats per minute, and
the respiratory rate 18 breaths per minute. The blood pressure was
130/75 mm Hg, and the oxygen saturation was 99 percent while the
patient was breathing ambient air.
On physical examination, the patient was thin but did not appear
acutely ill. No jaundice, rash, or scleral icterus was seen.
Shotty anterior cervical lymph nodes were palpated. The oropharynx
and lungs were normal. A grade 1 systolic ejection murmur was present
along the left sternal border. The abdomen was distended, and the
navel protruded; a nontender liver edge descended to the pelvic brim
and crossed the midline, and the splenic tip was 5 cm below the left
costal margin; no shifting dullness was found. There was tenderness
over the proximal portion of the right femur but not over the right
hip and knee; there was full range of passive motion of the knee and
hip, although knee extension was painful. No erythema or local warmth
was noted, and the knee was not swollen. The sensation of a light
touch was preserved, and motor power was intact, except that the leg
pain was severe enough that the patient would not voluntarily
move the right knee and declined to have her gait tested. Neurologic
examination revealed no evidence of extraocular eye-movement
abnormalities, ataxia, cognitive difficulties, or other abnormalities.
The urine had a specific gravity greater than 1.030 and was
positive (+) for protein and trace-positive for ketones. Laboratory
values are reported in. There was microcytosis (+++) with
anisocytosis (+); the white cells were normal. Hemoglobin
electrophoresis showed 62 percent hemoglobin A and 35 percent
hemoglobin C. The levels of urea nitrogen, creatinine, uric acid,
conjugated and total bilirubin, calcium, magnesium, and alkaline phosphatase
were normal.

Radiographs
of the right femur, hip, and lower right leg were unremarkable. A
radiograph of the chest obtained while the patient was supine
revealed that the lungs and pleural spaces were clear and that the
mediastinal contours and bones were normal. A computed tomographic
(CT) study of the abdomen and pelvis, performed after the intravenous injection of
contrast material, disclosed patchy sclerosis in the left femoral
head, suggesting avascular necrosis. A moderately large effusion was
present in the right hip joint, and the bone marrow had the density
of soft tissue rather than fat, indicating replacement of the marrow
fat by an infiltrate. There was marked hepatosplenomegaly, and
several retroperitoneal lymph nodes larger than 1 cm in diameter were
visible. The gallbladder, kidneys, pancreas, adrenal glands,
and large and small bowel were unremarkable.
abdomen and pelvis, performed after the intravenous injection of
contrast material, disclosed patchy sclerosis in the left femoral
head, suggesting avascular necrosis. A moderately large effusion was
present in the right hip joint, and the bone marrow had the density
of soft tissue rather than fat, indicating replacement of the marrow
fat by an infiltrate. There was marked hepatosplenomegaly, and
several retroperitoneal lymph nodes larger than 1 cm in diameter were
visible. The gallbladder, kidneys, pancreas, adrenal glands,
and large and small bowel were unremarkable.
A magnetic resonance imaging (MRI) study of the pelvis and femurs
showed a moderate effusion in the right hip and abnormal
enhancement in the synovium and soft tissues surrounding the proximal
portion of the right
 femur
and hip. T2-weighted and short tau inversion-recovery
images revealed edema in the soft tissues around the right hip. (The
short tau inversion-recovery technique suppresses the high-signal
intensity from fat and is useful in displaying fluid.) T1-weighted
images disclosed a uniformly low signal intensity in both femurs, the
pelvis, and imaged areas of the spine. No evidence of osteomyelitis
or knee joint effusion was detected. There was faint abnormal
enhancement of bone marrow in the proximal right femoral diaphysis,
and the marrow appeared brighter than muscle on the special images, a
finding believed to be indicative of bone marrow edema. A sharp zone
of transition in the femoral shaft, between enhancing marrow distally
and nonenhancing marrow proximally, suggested the possibility of an
extensive bone infarct within the proximal right femur.
femur
and hip. T2-weighted and short tau inversion-recovery
images revealed edema in the soft tissues around the right hip. (The
short tau inversion-recovery technique suppresses the high-signal
intensity from fat and is useful in displaying fluid.) T1-weighted
images disclosed a uniformly low signal intensity in both femurs, the
pelvis, and imaged areas of the spine. No evidence of osteomyelitis
or knee joint effusion was detected. There was faint abnormal
enhancement of bone marrow in the proximal right femoral diaphysis,
and the marrow appeared brighter than muscle on the special images, a
finding believed to be indicative of bone marrow edema. A sharp zone
of transition in the femoral shaft, between enhancing marrow distally
and nonenhancing marrow proximally, suggested the possibility of an
extensive bone infarct within the proximal right femur.
The patient's pain was relieved by administration of a potent analgesia.
Each day during hospitalization, the temperature rose as high
as 37.4°C but was normal at times. Antibiotic therapy was not given.
A urine culture yielded a few mixed bacteria, and a blood culture was
sterile. The results of additional tests were pending.
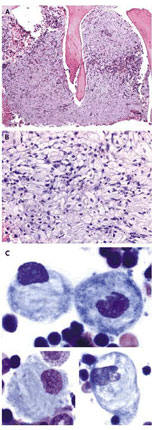
Results of bone marrow biopsy and aspiration
Which diagnostic
procedure must be performed?
What is the patient's possible diagnosis?




