|
پروفسور محمد
حسین سلطان زاده
استاد دانشگاه علوم پزشکی شهید بهشتی
متخصص کودکان ونوزادان
طی دوره بالینی عفونی از میوکلینیک آمریکا
دبیر برگزاری کنفرانس های ماهیانه گروه اطفال
دانشگاه علوم پزشکی شهید بهشتی
|
معرفی : دکتر فریبا
شیروانی
فوق تخصص عفونی اطفال
به اتفاق اعضای هیئت علمی گروه کودکان
بیمارستان امام حسین
|
تشخیص
Urine 24 hours
Volume 600 cc
Calcium
29mg/24hrs
50-300
Phosphorus
138
mg/24hrs 40-100
Na
51meq/24hrs 130-260
K
36meq/24hrs 40-80
Cl
55mmol/24hrs 110-250
Protein 108mg/24hrs
20-150
Citrate
38mg/24hrs 296.8 - 911.6
Oxalate 40mg/24hrs
male=29-85
female=29-79
Creat. 126
mg/24hrs 600-1800
Bone marrow result
Diagnosis:
Bone marrow aspiration
Some leishman body organism
identified in the background
Bone marrow biopsy
Visceral leishmaniasis
 |
 |
 |
 |
|
Closer view from previous image
|
Microscopic appearance of bone marrow aspiration * 40
Hyperplasic bone marrow full of precursors between bony spicles
|
 |
 |
|
Leishman bodies are in the macrophage and scattered in marrow field |
|
| |
 |
| |
Atlas view of leishman bodies in macrophages |
Differential diagnosis
Infectious causes
Subacute infectious endocarditis
Tuberculosis
Typhoid fever(prolonged salmonella
bacteremia)
brucellosis
typhus
Chronic Malaria
Amebic liver abscess
Hepatosplenic schistosomiasis
Disseminated fungal
infection:histoplasmosis
Infectious mononucleosis
Hematologic causes
Hodgkin disease
acute aleukemic leukemia
aplastic anemia
Etiology of stone formation
1- endemic stones(bladder stone)
2 – metabolic disorders
Hypercalciuria
Hyperoxaluria
Hyperuricosuria
Cystinuria
Xanthinuria,ect.
3- decrease of inhibitors
Citrate
Magnesium
Pyrophosphate
Glycosaminoglycan
Nephrocalcin
Osteopontine
Protrombin fragment-1
4- disease related
Prematurity
IBD
CF
RTA
MSK
ADPCK
GSD1
Cystinosis
antibiotics
5- infection
Urease positive
Corinebacterium urealiticum
6- anatomical disorders
Congenital anomalies
Foreign body
Surgical
7- medication
Drugs and metabolites
Metabolic effects
Treatment
Diet
Hydration
Medication
Surgery
Visceral leishmaniasis
Etiologic agents: leishmania
donovani,leishmania infantum/leishmania chagasi
Sometimes cutaneous leishmaniasis /
amazoneinsis and tropic can be visceral
Variation in intensity of involvement
One extreme
In apparent , self resolving
Ratio of 6.5/1 to 18/1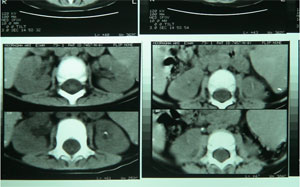
Classic (kala-azar)(dumdum – assam –
infantile splenomegaly)
Fever,weight loss,hepatosplenomegaly,
anemia ,leukopenia, trombocytopenia, hypergamaglobulinemia and in indian ,
hyperpigmentation
A small percentage of patients who
have been treated for VL will have diffuse skin lesions called post kalaazar
dermal leismaniasis
Hypopigmented,erythematous and nodular
on face and troso and persists for several months and years.
Epidemiology
90% in india,bangladesh,sudan,brazil
L. donovani is responsible for
visceral leishmaniasis in eastern india
and bangladesh
L. chagasi for Visceral leishmaniasis
in latin america
L. lnfantum is endemic in
mediterranean region
L. tropica in middle east
Transmission
Vector=sand fly (phlebotomus
argentipes)
Suitable reservoir= human , dogs ,
rats , gerbiles , small carnivores
Susceptible human
Other routes
Contaminated blood
Accidental needle stick
Sharing of contaminated needle
prenatal
Pathogenesis
Environmental and genetic
characteristics of host determines
severity of his disease
Components of immunity involvement in
kala-azar
Leishman specific CD4 t CELLS ☻
T helper cells that secret INF GAMA
and interleukin-2☻
IL10,IL4,TGF- BETA
INCUBATION PERIOD
3-8 months or longer than a year to 10
years
reactivation years after treatment may
occur
Clinical manifestation
Fever( intermittent , twice daily )
weight loss, cachecsia
Abdominal enlargement due to
hepatosplenomegaly and insidious
Rare cases with chill not rigor
Skin is dry and thin and scaly and
hair may be lost and hyperpigmentation
Extremities edema is in malnourished
children and echymosis
Epistaxis and gingival bleeding
hemorrage
Renal complications
microscopic hematuria usually mild
albuminuria
albuminuria of leishmaniasis is due
to focal leishmanial lesions, analogous to focal nephritis in bacteremias, and
not to fever. In fatal cases, parasitized macrophages may be seen in the
interstitial tissues of the kidneys.
chronic renal insufficiency during
convalescence from kala-azar, presumably from toxic effect of pentavalate
antimonates.
renal involvement
The kidney lesions are characterized
more by interstitial damage than glomerular or vascular damage.
nephrotic syndrome associated with
heavy proteinuria
The renal biopsy revealed a segmental
necrotising glomerulonephritis with 70% crescents.
In human VL, glomerulosclerosis,
mesangial cell proliferation, and interstitial nephritis have been reported
Advanced visceral leishmaniasis
Secondary bacterial infection
Pneumonia
Septicemia
Tuberculosis
Dysentery
measles
Visceral leishmaniasis in HIV
Splenomegaly may be absent
Patients may have involvement of lung
, pleura ,oral mucosa , esophagus , stomach , small intestine , skin , bone
marrow , aplastic anemia
Diagnosis:
Clinical
The diagnosis of leishmaniasis is
suggested by a history of possible exposure in endemic areas and by such
clinical manifestations as
(1) prolonged intermittent fever,
frequently with double daily peaks;
(2) enlargement of the spleen or
lymph nodes or both with, in some cases, enlargement of the liver;
(3) leukopenia;
(4) anemia; and
(5) elevation of serum globulin
Confimation
Splenic and lymph node aspiration and
biopsy and wright-giemsa stain
Culture of splenic and bone marrow
aspiation or blood in N.N.N media
Serum antibody
ELISA using recombinant k39 a kinesin-like
antigen
Leishmanin skin test(montenegro)
Is negative in visceral leishmaniasis
and has epidemiologic importance
laboratory
Anemia may be sever
Hemolysis,marrow replacement,splenic
sequestration of erythrocytes,hemodilution,TNF ALFA
Leukopenia
Hypergamaglobulinemia(Alb<3 and IgG >5
or 5-10bg/dl)
ESR usually elevated
Elevated liver transaminases
Mostly Kidney shows immune complex
deposition (mild glomerulonephritis)
Treatment:
Liposomal amphotericin (ambisome) can
be the choice
3mg kg /1,5,14,21 days
Adverse effect:fever,loss of
appetite,hypokalemia,azotemia,renal tubular acidosis trombophlebitis,weight loss
,hearing loss,diplopia,seizure, peripheral neuropathy,anaphylactic reaction
Amphotericine B deoxycolate is another
choice
Pentavalent antimony can still be used
but is not recommended in india because of 40% resistance
Adverse effects are abominal
pain,anorexia,vomiting,nausea,myalgia,arthralgia,headache,malaise,pancreatitis,renal
failure,ECG abnormalities
Pentamidine isethionate
2-4mg/kg for 15 days
Adverse effects:Life threatening
hypoglycemia by pancreatic beta cell injury
Miltefosine (phosphocoline analogue)
2.5 mg/kg/day for 4 weeks
Parenteral parmomycin
Ketoconazole,imidazole,itraconazole
Prevention of renal damage
Use of allopurinol in cannine
leishmaniasis prevented the progression of renal damage by improvement of
proteinuria and azoemia
It is used with pentavalent
antimonials
Response to therapy
Return of temperature to normal
Brisk reticulocytosis
Gradual reduction of spleen size
Reappearance of eosinophiles in
peripheral blood smear
Follow up:
Monitor every 6 months for 2 years
Antibody is absent 1 year later
If post kala_azar dermal leishmaniasis
occur treatment should be reinstituted
Thank you any comments
Fuadin (stibophen). All were
ultimately treated with Neostam (stibamine glucoside), Neostibosan (ethylstibamine),
or stibanose (sodium antimony gluconate, 20 mg. antimony per centimeter) in one
or more courses of one or more of these pentavalent compounds. Two failures were
re-treated, successfully, with stilbamidine (4, 4’-diamidinostilbene isethionate).
tartar emetic (potassium or sodium
antimony tartrate) may be attempted. A satisfactory dose schedule is as follows:
First day, 10 cc. of freshly prepared 0.5 percent solution; third day, 20 cc.;
fifth day, 30 cc., and this repeated every other day until a total of 360 cc.
(1.8 gm.) has been given.
Neostam 5.0 and
Neostibosan 10.0 gm
stilbamidine 4.0 gm.




