A Very Rare Form of
Bacterial Meningitis: Case Report
1-Prof.MohammadHossein Soltanzadeh MD,ID
2- Prof. Ahmad Siadati MD,ID
3- Dr. Fatemah Ashrafi , MD
Introduction:
Bacterial meningitis is a very serious fatal disease that is
caused by various microorganisms including bacterial agents.
Bacterial meningitis is associated with a very high rate of
mortality and morbidity in children and infants. Early prompt
diagnosis decreases this rate to about 2-5%. Most fatalities
occur in pneumoccal meningitis. Severe neurological disabilities
occur in 10-20% of the cases. Deafness is seen in 50% of the
patients (30% pneumoccal meningitis, 10% meningococcal and 5-20%
in H.influenza -type b- meningitis). Unfortunately 30% of
newborn succumb to death as a result of this disease. (Ref.
1,2,3,5 )
1-
Professor of Pediatrics Shahid Beheshti University of
Medical Science, Tehran .IRAN, ID from Mayo Clinic USA
2-
Professor of Pediatrics, Tehran University of Medical
Science, Tehran , IRAN, Research center of pediatrics ID
,Central Children Hospital
3-
Clinical Laboratory Specialist , Tehran Rsalat Hospital ,
Tehran , IRAN
Case Presentation:
The infant was an 11 months old girl weighing 9.2 kg.
She was admitted with the chief complaint of fever (39 °C)
that had started 5 days prior to admission. There was history of
a minor head trauma. 10 days before the admission.
On admission, CBC was sent to the laboratory; the results of
which are:
WBC=8800/mm3 (42% poly, 58% lymph)
Hb= 10.9 g/dl, ESR=121, CRP=1+
Ca= 8.8 mg/dl
Blood sugar=151 mg/dl
Platelets 230000/ mm3
U/A= Normal
BUN=20 mg/dl
Creatinine= 0.5 mg/dl
Figure (1)

However because of the high fever and ESR level, LP was
performed. The laboratory report of the CSF was as:
Sugar=25mg/dl
Protein=52mg/dl
WBC=62000(90% poly, 10%
lymph)
RBC=300
CSF smear= Gram positive
CSF culture=Pneumococcus
Blood Culture= Negative
U/C = Negative
Diagnosis:
This was a very rare and
possibly a one-of-a-kind form of Bacterial Meningitis with WBC
in CSF of 62000 .
Treatment was initiated with Ceftriaxone ( 50 mg/kg/dose every
12 hrs), Vancomycin ( 15 mg/kg/dose) and Dexamethasone.
The patient underwent brain CT scan on the third day of
operation. The report was:
Subdural effusion with few isodense areas in both frontal lobes.
Figure (2)
Four days after admission another CBC was done which showed:
WBC=19600( 73% poly, 26% lymph)
Platelet= 507000/mm3
ESR=82
-
Ninth day of admission, LP was done which showed:
WBC=100
Protein=25
Sugar=45
-
Twelfth day CBC showed:
WBC=20700/mm3 (80% poly, 18% lymph, 2% band)
Hb= 9.4 g/dl,
ESR=135,
CRP=2++
The patient underwent a second brain CT scan on day 14 of
treatment. Brain scan reported: There is evidence of abnormal
frontal lobe bilaterally more prominent on the left side. Fluid
collection with mild mass effect in left frontal area (epidural
empyema).
Figure (3)
Figure(4)
Therefore considering the hyperleucocytosis polynucleosis, ESR
135 and CSF cell count =100,
Atypical Kawasaki's
Disease-a form of vasculitis-was considered as diagnosis
for the patient; as a result of which she was put on IVIG(
2gr/kg) and Aspirin (100mg/kg) for two weeks.
Meanwhile ABR was done: for left ear 20 dbH
Figure (5)
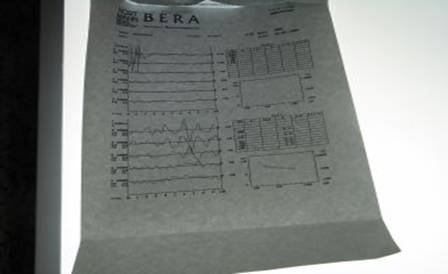
l and right ear 110dbHl was recorded. All other investigations
including abdominal sonography, echocardiography and
opthalamoscopy were normal.
After two weeks of aspirin consumption the dose was reduce to
100 mg/day and continued for 3 months.
-Thirty six days after treatment, CBC was:
WBC= 8100/mm3 (31% poly, 66% lymph)
Platelet=370000
Hb=11.9gr/dl
ESR=44
CRP=Negative
-Forty seven days after treatment, CBC was:
WBC=8500 (31% poly, 67% lymph)
ESR=13
Platelet=340000
CRP=Negative
Figure (6)

Figure (7)

Figure (8)

After 4.5 months of treatment: laboratory findings and brain
CTscan had become normal.
Figure(9)

Figure (10)
Figure (11)

Figure ( 12 )

Discussion
Streptococcus pneumoniae has
been dramatically altered by the use of vaccine in February
2000 risk factors include : otitis media , sinusitis ,
pneumonia . ( Ref. 3,4 )
Diagnosis of acute bacterial
meningitis is confirm by analysis of the CSF
Complications include seizure ,
increased ICP , cranial nerve palsies , stroke , cerebral
herniation and thrombosis . (Ref. 1,5 )
Collections of fluid in the
subdural space develop in 10-30 % of patients . CT and MRI
scanning confirms the presence of a subdural effusion that
should be treated by aspiration .
Fever usually resolved within
5-7 days of the onset of therapy . prolonged fever > 10 days is
noted in about 10% of patients due to Nosocomial or secondary
infection. ( Ref. 2 )
Kawasaki Disease (KD) is a
systemic vasculitis that occurs most commonly in children less
than 5 years . ( Ref. 5 ) Most cases of KD occur in children
younger than 12 years of age. in 1967 Tomisaku Kawasaki
developed diagnostic criteria for an apparently new illness .The
illness is characterized by fever and the following clinical
feature (1) bilateral bulbar conjunctival injection without
exudates (2) erythematous mouth and pharynx, strawberry tongue
,and red ,cracked lips (3) a polymorphous , generalized ,
erythematous rash that can be morbilliform , maculopapular or
scarlatiniform or may resemble erythema multiform (4) changes in
the peripheral extremities consisting of induration of the hands
and feet with erythematous palms and soles, often with later
priunguinal desquqmation and (5) acute , nonsupurative , usually
unilateral, cervical lymph – adenopathy with at least one node
1.5 cm in diameter. For diagnosis of classic KD patient should
have fever at least 4 days and at least 4 of these 5 features
without alternative explanation for the findings .other finding
10%-20% meningismus with CSF pleocytosis . ( Ref. 5,6,7 )
Incomplete KD can be diagnosed
. Incomplete KD is mor common in infants younger than 12 months
of age than in older children ( Ref . 8 )
REFERENCES
1 – Bonsu BK ,Harper MB: fever
interval before diagnosis ,prior antibiotic treatment , clinical
outcome for young children with bacterial meningitis , clin
infect Dis 2001;32.566-572
2 - Kilpi T , Anttila M,Kallio
MJ ,et al ; Lent of prediagnostic history related to the course
and sequelae of childhood bacterial meningitis .pediatr infect
Dis j 1993;12;184-188
3 – McIntyre PB ,Macintyre CR
,Gilmour R, et al; A population based study of the impact of
corticosteroid therapy and delayed diagnosis on the outcome of
childhood pneumococcal meningitis . Arch Dis Child
2005;90;391-396.
4 – Tunkel AR , Hartman BJ
,Kaplan SL,et al; practice guideline for the management of
bacterial meningitis. Clin infect Dis 2004;39;1267 – 1284
5- Larry K Pickering ,MD, FAAP,
Associate Editor- David W ,Kimberlin , MD, FAAP ,Associate
Editor – Sarah S, Long ,MD , FAAP, Associate Editor , Report of
the Committee on Infectious Diseases 2009
6- Anderson MS Todd JK ,Glode
,MP ,Delayed diagnosis of Kawasaki Syndrome , An analysis of
the problem , Pediatrics 2005
7- Muta H,Ishii ,M, Egami K, et
al , Early intravenous gamma – globulin treatment for Kawasaki
Disease; The The nationwide surveys in Japan ,J Pediatr 2004
7- Newburger , JW , M , Gerber
MA , et al : Diagnosis , Treatment and long-term management of
Kawasaki Disease : Pediatrics 2004
8 – Shulman ST , Rowley AH ,
Advance in Kawasaki Disease , Eur J Pediatr , 2004



